Latest News

UMass student group declares no confidence in chancellor
AMHERST — A day after 132 people were arrested in pro-Palestinian protests on the University of Massachusetts campus, the university’s student government Wednesday night formally declared it had no confidence in Chancellor Javier Reyes and his...

‘Knitting treasure’ of the Valley: Northampton Wools owner spreads passion for ancient pastime
NORTHAMPTON — Above the rows of shelves at Northampton Wools, amid all of the yarn of different colors, materials and thickness that fill every cubby in sight, sits a famous sweater worn by Charlize Theron in the Academy Award-winning film “The Cider...
Most Read
 More than 130 arrested at pro-Palestinian protest at UMass
More than 130 arrested at pro-Palestinian protest at UMass
 Public gets a look at progress on Northampton Resilience Hub
Public gets a look at progress on Northampton Resilience Hub
 Northampton bans auto dealerships near downtown; zone change won’t affect Volvo operation on King Street
Northampton bans auto dealerships near downtown; zone change won’t affect Volvo operation on King Street
 UMass basketball: Bryant forward Daniel Rivera to be Minutemen’s first transfer of the offseason
UMass basketball: Bryant forward Daniel Rivera to be Minutemen’s first transfer of the offseason
 Town manager’s plan shorts Amherst Regional Schools’ budget
Town manager’s plan shorts Amherst Regional Schools’ budget
 Police respond to alcohol-fueled incidents in Amherst
Police respond to alcohol-fueled incidents in Amherst
Editors Picks
 A Look Back, May 9
A Look Back, May 9
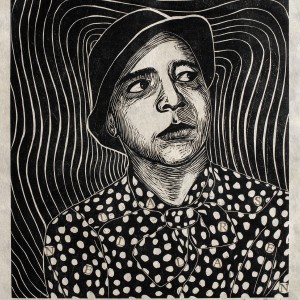 Overlooked no more: Leverett artist’s woodcut prints celebrate remarkable women of the past
Overlooked no more: Leverett artist’s woodcut prints celebrate remarkable women of the past
 Karen Gardner: We all deserve a break
Karen Gardner: We all deserve a break
 Arts Briefs: Dance festival and a one-woman play in Northampton, summer music fests in Easthampton, and more
Arts Briefs: Dance festival and a one-woman play in Northampton, summer music fests in Easthampton, and more
Sports

Boys volleyball: Granby cruises to 3-0 sweep over Athol (PHOTOS)
GRANBY – Michael Swanigan and Braeden Gallagher had just taken the volleyball net down from another win Wednesday night, but they weren’t ready to pack up the balls just yet.The two went off to the side of the gym and began hitting at each other,...
Opinion

Martha Jorz: Stop supporting UMass and Raytheon
To those protesting the war and genocide in Gaza, refusing to support those institutions with monetary gifts is also an option. If we stop financially supporting and investing in those institutions that make the production of weapons of war possible...
 Tony Giardina: Faith and inclusion
Tony Giardina: Faith and inclusion
 John Frey: School Committee must practice prudent fiscal management
John Frey: School Committee must practice prudent fiscal management
 Doron Goldman: Israel's situation is complicated
Doron Goldman: Israel's situation is complicated
 Jeanne Horrigan: Amherst seniors grateful for ARPA support
Jeanne Horrigan: Amherst seniors grateful for ARPA support

Business

Area property deed transfers, May 2
AMHERST Faheem Ibrahim Lt and Faheem Ibrahim to Nan Zhao and Zhihong Ni, 16 Arbor Way, $738,000 Richard B. Spurgin to Yg Pleasant LLC, East Pleasant Street, Lot 1, $218,000 Richard B. Spurgin to Yg Pleasant LLC, East Pleasant Street, Lot 2,...
Arts & Life

Speaking of Nature: Capturing my Bermuda nemesis: The Great Kiskadee nearly evaded me, until I followed its song
We’ve reached that point in the school year when it is actually painful (I mean physically painful) for me to leave my yard in the morning. May is the true month of the reawakening and blooming of Nature’s splendor and last week she was in full...
Obituaries
 Eli Knapp Abrams
Eli Knapp Abrams
Florence, MA - Eli Knapp Abrams, of Florence Massachusetts, passed away suddenly on Monday, April 22nd, 2024 in Goshen, MA. Eli was born in Beverly, MA on March 19th, 2003. He is the cherished son of Jennifer and Maury Abrams, and belov... remainder of obit for Eli Knapp Abrams
 Lori E. Christenson
Lori E. Christenson
Winston-Salem, NC - To my family and friends: With great sadness, I wish to announce the passing of Lori Christenson, my beloved wife of 40 years, who died peacefully at our home in Winston-Salem, North Carolina on February 20th, 2024. ... remainder of obit for Lori E. Christenson
 Helen Czelusniak
Helen Czelusniak
South Kingstown, RI - Helen A. (Fil) Czelusniak formerly of Easthampton, died on March 22, 2024 at South County Hospital in South Kingstown, RI. Born in Hadley, she was 97 years old. Helen graduated from Hopkins Academy and Northampton... remainder of obit for Helen Czelusniak
 Wilford J. Morton Jr.
Wilford J. Morton Jr.
Wilford J. Morton, Jr. Belchertown, MA - Wilford J. Morton, Jr., beloved husband, father, and friend, passed away peacefully on April 14, 2024, at the age of 85. Wilford was born on September 17, 1938, in Waltham, Massachusetts, to his p... remainder of obit for Wilford J. Morton Jr.

 Columnist Olin Rose-Bardawil: American dream out of reach for many
Columnist Olin Rose-Bardawil: American dream out of reach for many
 VA preps for birthday bash: Leeds medical center to mark 100 with circus acts, games and visits by prominent leaders
VA preps for birthday bash: Leeds medical center to mark 100 with circus acts, games and visits by prominent leaders
 Chesterfield budget, up 4.5%, faces Town Meeting vote Monday
Chesterfield budget, up 4.5%, faces Town Meeting vote Monday
 No contested seats in Southampton election May 21
No contested seats in Southampton election May 21
 Health board seat sole contested race in Pelham election Tuesday
Health board seat sole contested race in Pelham election Tuesday
 Area briefs: Walk for peace in Gaza; high blood pressure support group forms; Velis honor work recovery work
Area briefs: Walk for peace in Gaza; high blood pressure support group forms; Velis honor work recovery work
 Guest columnist Josh Silver: Northampton school budget — Let’s start with kindness, accuracy and respect
Guest columnist Josh Silver: Northampton school budget — Let’s start with kindness, accuracy and respect
 With Jones project in question, Amherst won’t sign lease for temporary digs
With Jones project in question, Amherst won’t sign lease for temporary digs
 Amherst College faculty join students in urging divestment from military suppliers to Israel
Amherst College faculty join students in urging divestment from military suppliers to Israel
 Baseball: Hampshire, South Hadley to ‘get a little taste of what it’s like to be a pro’ at Dunkin’ Park
Baseball: Hampshire, South Hadley to ‘get a little taste of what it’s like to be a pro’ at Dunkin’ Park Belchertown Twirlers capture first place at Northeast Regional Championships
Belchertown Twirlers capture first place at Northeast Regional Championships UMass basketball: Minutemen nab another transfer in Arizona State forward Akil Watson
UMass basketball: Minutemen nab another transfer in Arizona State forward Akil Watson UMass basketball: Bryant forward Daniel Rivera to be Minutemen’s first transfer of the offseason
UMass basketball: Bryant forward Daniel Rivera to be Minutemen’s first transfer of the offseason Music key to Northampton’s downtown revival: State’s top economic development leader tours city
Music key to Northampton’s downtown revival: State’s top economic development leader tours city  Locking up carbon for good: Easthampton inventor’s CO2 removal system turns biomass into biochar
Locking up carbon for good: Easthampton inventor’s CO2 removal system turns biomass into biochar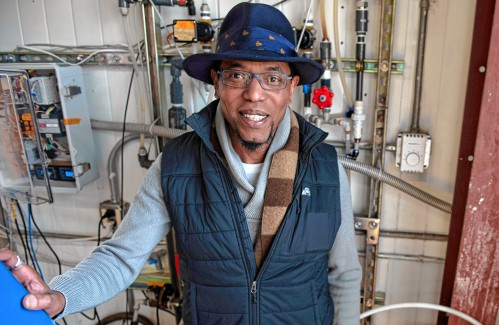 Advancing water treatment: UMass startup Elateq Inc. wins state grant to deploy new technology
Advancing water treatment: UMass startup Elateq Inc. wins state grant to deploy new technology New Realtor Association CEO looks to work collaboratively to maximize housing options
New Realtor Association CEO looks to work collaboratively to maximize housing options Easthampton author Emily Nagoski has done the research: It’s OK to love your body
Easthampton author Emily Nagoski has done the research: It’s OK to love your body Earth Matters: Honoring a local hero: After 40 years, Hitchcock Center bids farewell to educator and creative leader, Colleen Kelley
Earth Matters: Honoring a local hero: After 40 years, Hitchcock Center bids farewell to educator and creative leader, Colleen Kelley Valley Bounty: Delivering local food onto students’ plates: Marty’s Local connects farms to businesses
Valley Bounty: Delivering local food onto students’ plates: Marty’s Local connects farms to businesses Let’s Talk Relationships: Breaking up is hard to do: These tools can help it feel easier
Let’s Talk Relationships: Breaking up is hard to do: These tools can help it feel easier
