Latest News
 Holyoke man finds bear paw in his yard
Holyoke man finds bear paw in his yard
 Prices up, sales down in early spring housing market
Prices up, sales down in early spring housing market

Petition to block auto dealership on King Street falters in Northampton
NORTHAMPTON — A joint meeting between the Northampton City Council’s Committee on Legislative Matters and the city’s Planning Board heard public comments on a petition to ban further automobile dealerships near the city’s downtown, an issue that...

Flair and flavor: Couple draws on European, regional travel and food expertise to bring gourmet Aster + Pine Market to Amherst
AMHERST — From their own journeys in Europe and across New England and the Northeast, and their experience in the hospitality industry, a Northampton couple is creating a market featuring wines, pantry staples and fresh, local produce in downtown...
Most Read
 Holyoke man finds bear paw in his yard
Holyoke man finds bear paw in his yard
 Boyfriend accused in slaying of Hampden sheriff’s assistant, former legislator’s top aide
Boyfriend accused in slaying of Hampden sheriff’s assistant, former legislator’s top aide
 Three finalists named for Ryan Road School principal in Northampton
Three finalists named for Ryan Road School principal in Northampton
 Developer pitches new commercial building on Route 9 in Hadley
Developer pitches new commercial building on Route 9 in Hadley
 Two men dump milk, orange juice over themselves at Amherst convenience store
Two men dump milk, orange juice over themselves at Amherst convenience store
 Sadiq to leave Amherst middle school principal role
Sadiq to leave Amherst middle school principal role
Editors Picks
 A Look Back: April 18
A Look Back: April 18
 Spring brings new art: A look at what's on tap in April at selected local galleries
Spring brings new art: A look at what's on tap in April at selected local galleries
 News Briefs: Roadwork in Plainfield; bake sale in Hadley
News Briefs: Roadwork in Plainfield; bake sale in Hadley
 LIME SPREADER
LIME SPREADER
Sports

High schools: Offense on fire for Granby girls lacrosse in 20-2 win over McCann Tech
Fourteen first-half goals helped the Granby girls lacrosse team to a dominant 20-2 victory over McCann Tech on Wednesday afternoon.Eleven different players recorded goals in the win.Brenna Moreno’s four goals and Kalli White’s hat trick led the way...
 Baseball: Chicopee Comp strikes early, takes down Amherst (PHOTOS)
Baseball: Chicopee Comp strikes early, takes down Amherst (PHOTOS)
 Florence’s Gabby Thomas gearing up for 2024 Paris Olympics
Florence’s Gabby Thomas gearing up for 2024 Paris Olympics
 Jiri Smejkal gets 1st goal, Senators beat Bruins 3-1 in regular-season finale
Jiri Smejkal gets 1st goal, Senators beat Bruins 3-1 in regular-season finale
 High schools: Belchertown, Easthampton split dual track meet (PHOTOS)
High schools: Belchertown, Easthampton split dual track meet (PHOTOS)
Opinion

Guest columnist Mariel E. Addis: Under seige from all sides
When I first heard John Lennon’s masterpiece “Imagine,” and heard the line “imagine no religion,” I thought, “How awful is that; religion is a good thing!” Probably in junior high at the time, I couldn’t understand the significance of the line. I do...
 Julia Riseman: Join Friends of Northampton Trails
Julia Riseman: Join Friends of Northampton Trails
 Shelly Berkowitz: More examples of corporate greed
Shelly Berkowitz: More examples of corporate greed

Business

Area property deed transfers, April 18
AMHERST 44 Chapel Rd, $560,750, B: Kristin M. Flewelling and Christine L. Larson, S: Paul A. Schroeder and Maria Monasterios BELCHERTOWN 203 South St, $507,150, B: Glenna J. Young, S: M & F Land Dev LLC 45 West St, $200,000, B: Serenity Ft and...
 Tea Guys of Whately owes $2M for breach of contract, judge rules
Tea Guys of Whately owes $2M for breach of contract, judge rules
Arts & Life

Speaking of Nature: Indulging in eye candy: Finally, after such a long wait, it’s beginning to look like spring is here
I have just about reached the end of my patience with the winter of 2024. I realize that this may sound a bit strange, especially because we are now in the beginning of spring, but those of us who bore the brunt of the April snowstorm may sympathize...
Obituaries
 Garry Tudryn
Garry Tudryn
[IMAGE]GARRY TUDRYN HATFIELD, MA - Garry Morrison Tudryn, 67 of West Street in Hatfield, passed away April 13, 2024 at the Care One Nursing and Rehab Center in Northampton. Born in Northampt... remainder of obit for Garry Tudryn
 Jacques Ben Abbes
Jacques Ben Abbes
HADLEY, MA - Jacques Ben Abbes, leaves his wife, Ngoc Anh Tran. Children; Vincent Tran (Nhu Nguyen) and Jacqueline Ben Abbes (Victor Loye) Grandchildren, Benjamin and Scott Tran. CALLIN... remainder of obit for Jacques Ben Abbes
 Geraldine Packard
Geraldine Packard
Northampton, MA - Geraldine Packard, 87, passed away at her home in Northampton on April 13, 2024. Born to Curtis and Mildred (Smith) Chase on September 23, 1936 in Wolfeboro, New Hampshire... remainder of obit for Geraldine Packard
 Russell E. Lent Sr.
Russell E. Lent Sr.
[IMAGE]Russell E. Lent, Sr. Easthampton, MA - Russell Eugene Lent, Sr. 89, longtime resident of Easthampton, passed away peacefully on Friday April 12, 2024, at his home. Born in Coshocton, ... remainder of obit for Russell E. Lent Sr.

 Columnist Johanna Neumann: Reaping the rewards of rooftop solar
Columnist Johanna Neumann: Reaping the rewards of rooftop solar
 Amherst Fire Chief Walter ‘Tim’ Nelson to retire in June
Amherst Fire Chief Walter ‘Tim’ Nelson to retire in June
 First look at how little Amherst’s police alternative being used called troubling
First look at how little Amherst’s police alternative being used called troubling
 Mass. saw nearly 200 percent rise in antisemitic incidents last year
Mass. saw nearly 200 percent rise in antisemitic incidents last year
 Guest columnist Jim Palermo: Beware the zeitgeist! It’s bad for our kids
Guest columnist Jim Palermo: Beware the zeitgeist! It’s bad for our kids
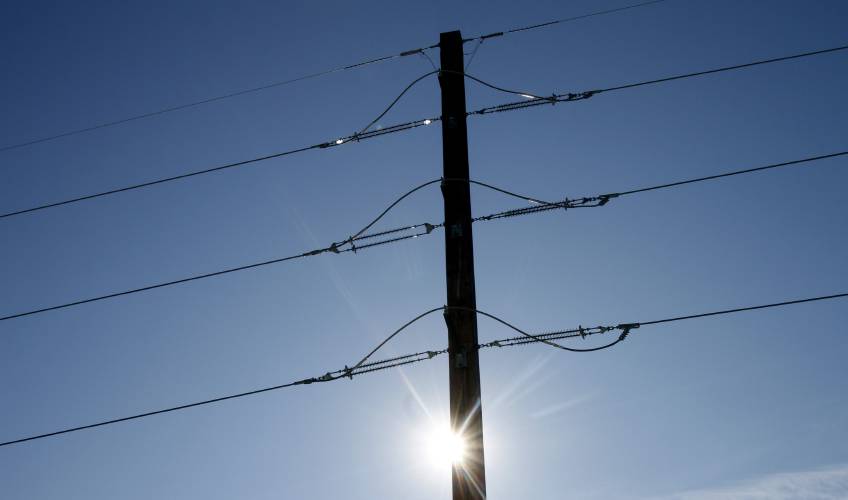 Justine McCarthy and Ed Lamoureux: Political will needed to benefit from new power line technology
Justine McCarthy and Ed Lamoureux: Political will needed to benefit from new power line technology Maggie Baumer: Access to prosthetics and orthotics for physical activity a right, not a privilege
Maggie Baumer: Access to prosthetics and orthotics for physical activity a right, not a privilege Recognizing an ‘inspiring force’: City business owner honored with Black Excellence award
Recognizing an ‘inspiring force’: City business owner honored with Black Excellence award Consumer Corner with Anita Wilson: A two-day reprieve in tax filing deadline offers time for tips
Consumer Corner with Anita Wilson: A two-day reprieve in tax filing deadline offers time for tips Sublime Systems lands $87M federal award for low-carbon cement plant in Holyoke
Sublime Systems lands $87M federal award for low-carbon cement plant in Holyoke Weekly Food Photo Contest: This week’s winner: Nicholas Horton of Northampton
Weekly Food Photo Contest: This week’s winner: Nicholas Horton of Northampton What does freedom look like today? On view at Williams College, seven Black American artists interpret the meaning of emancipation
What does freedom look like today? On view at Williams College, seven Black American artists interpret the meaning of emancipation Book Bag: ‘Dear Oliver: An Unexpected Friendship With Oliver Sacks’ by Susan B. Barry; ‘Benjy’s Messy Room’ by Barbara Diamond Goldin
Book Bag: ‘Dear Oliver: An Unexpected Friendship With Oliver Sacks’ by Susan B. Barry; ‘Benjy’s Messy Room’ by Barbara Diamond Goldin Only Human with Joan Axelrod-Contrada: To journal or not to journal: Advice for when journaling feels like it’s holding you back
Only Human with Joan Axelrod-Contrada: To journal or not to journal: Advice for when journaling feels like it’s holding you back
