Latest News

Upon Nancy’s Floor: 33 Hawley event celebrates iconic dancers, history, and a new dance floor
Among the many features that are part of 33 Hawley, the Northampton Community Arts Trust building that was finally completed in early January following 10 years of construction, there’s probably nothing more important to dancers than the floor of the...

Photos: Remembering the Armenian genocide
Most Read
 Treehouse, Big Brothers Big Sisters turn race schedule snafu into positive
Treehouse, Big Brothers Big Sisters turn race schedule snafu into positive
 Northampton man will go to trial on first-degree murder charge after plea agreement talks break down
Northampton man will go to trial on first-degree murder charge after plea agreement talks break down
 Area property deed transfers, April 25
Area property deed transfers, April 25
 Contentious dispute ends as Hampshire Regional schools, union settle on contract
Contentious dispute ends as Hampshire Regional schools, union settle on contract
 South Hadley’s Lauren Marjanski signs National Letter of Intent to play soccer at Siena College
South Hadley’s Lauren Marjanski signs National Letter of Intent to play soccer at Siena College
 Primo Restaurant & Pizzeria in South Deerfield under new ownership
Primo Restaurant & Pizzeria in South Deerfield under new ownership
Editors Picks
 Embracing both new and old: Da Camera Singers celebrates 50 years in the best way they know how
Embracing both new and old: Da Camera Singers celebrates 50 years in the best way they know how
 Time to celebrate kids and books: Mass Kids Lit Fest offers a wealth of programs in Valley during Children’s Book Week
Time to celebrate kids and books: Mass Kids Lit Fest offers a wealth of programs in Valley during Children’s Book Week
 Arts Briefs: A themed exhibit in Northampton, new opportunities for artists in Easthampton, and more
Arts Briefs: A themed exhibit in Northampton, new opportunities for artists in Easthampton, and more
 The Beat Goes On: Album release shows by Barnstar! and Lisa Bastoni, a Young@Heart Chorus concert with new special guests, and more
The Beat Goes On: Album release shows by Barnstar! and Lisa Bastoni, a Young@Heart Chorus concert with new special guests, and more
Sports

High schools: Northampton boys tennis takes down Amherst in rain-shortened title-game rematch (PHOTOS)
AMHERST – Amherst’s Miles Jeffries took the first set from Northampton’s Reilly Fowles on Wednesday afternoon, but rain shortened what had the potential to be the best boys tennis match of the season in Hampshire County. Amherst coach Kevin Jeffries...
 High schools: South Hadley baseball shakes off slow start, runs past Granby
High schools: South Hadley baseball shakes off slow start, runs past Granby
 Local briefs: Amherst Youth Baseball, Northampton Youth Softball
Local briefs: Amherst Youth Baseball, Northampton Youth Softball
 Girls lacrosse: Anna Puttick helps Hampshire take down Granby 13-9 (PHOTOS)
Girls lacrosse: Anna Puttick helps Hampshire take down Granby 13-9 (PHOTOS)
Opinion

Guest columnists Ellen Attaliades and Lynn Ireland: Housing crisis is fueling the human services crisis
Vacancies at programs operated by human services providers — despite some progress over the last two years — are still much too high. More than one in four direct support professional positions in adult residential and day programs for people with...
 Lora Sandhusen: Discourage ultra-wealthy consumption habits with carbon tax
Lora Sandhusen: Discourage ultra-wealthy consumption habits with carbon tax
 Guest columnist Jena Schwartz: Things I have not said
Guest columnist Jena Schwartz: Things I have not said
 Wendy Parrish: Northampton Volunteer Fair
Wendy Parrish: Northampton Volunteer Fair

Business
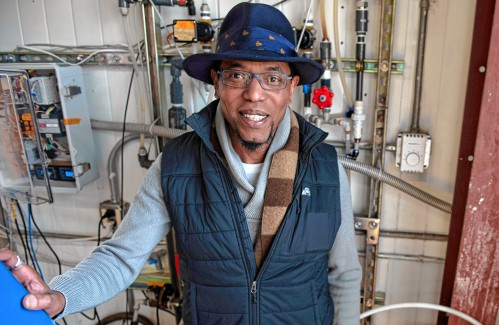
Advancing water treatment: UMass startup Elateq Inc. wins state grant to deploy new technology
AMHERST — In the four years since its founding on the UMass campus, startup Elateq Inc., a water treatment and hardware company, has landed contracts big (think PepsiCo) and small (think town of Amherst).Now the company, which uses advanced...
 New Realtor Association CEO looks to work collaboratively to maximize housing options
New Realtor Association CEO looks to work collaboratively to maximize housing options
 Area property deed transfers, April 25
Area property deed transfers, April 25
 Primo Restaurant & Pizzeria in South Deerfield under new ownership
Primo Restaurant & Pizzeria in South Deerfield under new ownership
 Petition to block auto dealership on King Street falters in Northampton
Petition to block auto dealership on King Street falters in Northampton
Arts & Life

Speaking of Nature: ‘Those sound like chickens’: Wood frogs and spring peepers are back — and loud as ever
During a recent lecture on evolutioin I had to explain the differences between three different processes known as geographic, temporal and behavioral isolation. Geographic isolation is the easiest of these concepts to understand because it involves...
Obituaries
 Eli Knapp Abrams
Eli Knapp Abrams
Florence, MA - Eli Knapp Abrams, of Florence Massachusetts, passed away suddenly on Monday, April 22nd, 2024 in Goshen, MA. Eli was born in Beverly, MA on March 19th, 2003. He is the cherished son of Jennifer and Maury Abrams, and belov... remainder of obit for Eli Knapp Abrams
 Donald E. Hooton
Donald E. Hooton
South Hadley, MA - South Hadley Donald E. Hooton, 91, passed away peacefully on Sunday, April 21 st , 2024, surrounded by his loving family. He was born in Holyoke to the late Eva (Utley) and Leonard Hooton. Donald moved to South ... remainder of obit for Donald E. Hooton
 Peter G. Tobin
Peter G. Tobin
Leeds, MA - Peter G. Tobin, 59, of Evergreen Rd. in Leeds passed away peacefully at his home on Tuesday, with his daughter Meghan and his former wife, Cathy Tobin at his side. Peter leaves his devoted daughter Meghan and his beloved cat... remainder of obit for Peter G. Tobin
 Doris Ilnicky
Doris Ilnicky
S. Hadley, MA - Doris M. Ilnicky, 76, of S. Hadley, passed away peacefully on Friday, April 12, 2024, with her daughter, son in law, and niece by her side. She was born February 26, 1948, in Northampton to the late Octave and Alice (Bai... remainder of obit for Doris Ilnicky

 Supreme Court seems skeptical of Trump’s claim of absolute immunity but decision's timing is unclear
Supreme Court seems skeptical of Trump’s claim of absolute immunity but decision's timing is unclear
 Hatfield eyes reserves to cover unexpected spike in payments to Smith Vocational
Hatfield eyes reserves to cover unexpected spike in payments to Smith Vocational
 Ashfield considers seeking ‘Climate Leader’ designation
Ashfield considers seeking ‘Climate Leader’ designation
 Building conversion, battery storage bylaws up for vote at Sunderland Town Meeting
Building conversion, battery storage bylaws up for vote at Sunderland Town Meeting
 Area briefs: Bonifaz to speak at Law Day events; Easthampton Film Festival preps for third year; Granby Candidates Night
Area briefs: Bonifaz to speak at Law Day events; Easthampton Film Festival preps for third year; Granby Candidates Night
 More arrested in pro-Palestinian campus protests ahead of college graduation ceremonies
More arrested in pro-Palestinian campus protests ahead of college graduation ceremonies
 Amherst regional superintendent candidate stresses collaboration, experience
Amherst regional superintendent candidate stresses collaboration, experience
 Columnist Carrie N. Baker: A moral justification for civil disobedience to abortion bans
Columnist Carrie N. Baker: A moral justification for civil disobedience to abortion bans
 William Strickland, a longtime civil rights activist, scholar and friend of Malcolm X, has died
William Strickland, a longtime civil rights activist, scholar and friend of Malcolm X, has died
 2024 Gazette Girls Indoor Track Athlete of the Year: Allie Sullivan, Northampton
2024 Gazette Girls Indoor Track Athlete of the Year: Allie Sullivan, Northampton Guest columnist Rob Okun: Still No. 1 in male mass shootings 25 years after Columbine
Guest columnist Rob Okun: Still No. 1 in male mass shootings 25 years after Columbine Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28
Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28 Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear
Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many
Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many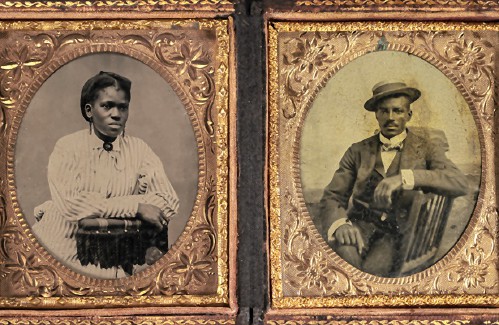 Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
