Latest News

LightHouse Holyoke to buy Gateway City Arts, expand offerings and enrollment at alternative school
HOLYOKE — After months of work on securing a new home elsewhere, LightHouse school plans to buy Gateway City Arts in a move that will allow the burgeoning alternative secondary school to meet its growing demand and expand its offerings.LightHouse...

Neighbors lifting neighbors: Demand at South Hadley’s food bank spiking as more families seek help
SOUTH HADLEY — Never go hungry.It’s the one rule that must not be broken at Neighbors Helping Neighbors, the organization that over the last 14 years has helped thousands of people from South Hadley and surrounding towns keep food on the table during...
Most Read
 South Hadley man fatally shot in attempted robbery
South Hadley man fatally shot in attempted robbery
 Smith College exhibit explores Sylvia Plath’s botanical inspiration
Smith College exhibit explores Sylvia Plath’s botanical inspiration
 Holyoke man finds bear paw in his yard
Holyoke man finds bear paw in his yard
 Guest columnist Bill Dwight: How to make sense of Northampton’s school budget dilemma
Guest columnist Bill Dwight: How to make sense of Northampton’s school budget dilemma
 South Hadley’s Lauren Marjanski signs National Letter of Intent to play soccer at Siena College
South Hadley’s Lauren Marjanski signs National Letter of Intent to play soccer at Siena College
 Deerfield residents petitioning to fix ‘dangerous’ intersection
Deerfield residents petitioning to fix ‘dangerous’ intersection
Editors Picks
 A Look Back: April 23
A Look Back: April 23
 Photos: Hangers for history
Photos: Hangers for history
 Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear
Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear
 The Beat Goes On: Album release shows by Barnstar! and Lisa Bastoni, a Young@Heart Chorus concert with new special guests, and more
The Beat Goes On: Album release shows by Barnstar! and Lisa Bastoni, a Young@Heart Chorus concert with new special guests, and more
Sports

Baseball: Northampton nearly comes all the way back before falling to Chicopee 15-14 (PHOTOS)
NORTHAMPTON — It looked like a comeback that would be talked about for years to come for the Northampton baseball team.Behind 14-5 entering the bottom of the sixth inning on their home field, the Blue Devils refused to roll over in the late stages of...
 High schools: Rosie Follet, Easthampton shut down Agawam in 3-1 win
High schools: Rosie Follet, Easthampton shut down Agawam in 3-1 win
Opinion

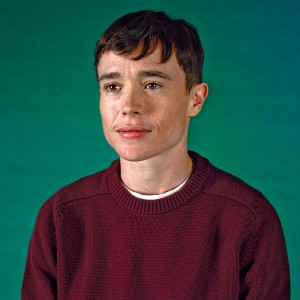
Guest columnist Oriel Strong: Think impossible thoughts
Mariel E. Addis’s April 17 guest column “Under siege from all sides” was heartfelt and thought-provoking. I share Addis’ foundational ethic that we must resist ranking any human being as better or worse than another. Trans and gender-nonconforming...
 Guest columnist Barry Hirsch: Palestinians should turn to Israel for real path to peace
Guest columnist Barry Hirsch: Palestinians should turn to Israel for real path to peace
 Patricia Crosby: Meeting of Friends call for an immediate cease-fire in Gaza
Patricia Crosby: Meeting of Friends call for an immediate cease-fire in Gaza
 Columnist Richard Fein: National debt — A threat to our nation’s future
Columnist Richard Fein: National debt — A threat to our nation’s future
 My Turn: The pecking order revolution: Massachusetts’ fight for animal rights
My Turn: The pecking order revolution: Massachusetts’ fight for animal rights

Business

Petition to block auto dealership on King Street falters in Northampton
NORTHAMPTON — A joint meeting between the Northampton City Council’s Committee on Legislative Matters and the city’s Planning Board heard public comments on a petition to ban further automobile dealerships near the city’s downtown, an issue that...
 Flair and flavor: Couple draws on European, regional travel and food expertise to bring gourmet Aster + Pine Market to Amherst
Flair and flavor: Couple draws on European, regional travel and food expertise to bring gourmet Aster + Pine Market to Amherst
 Prices up, sales down in early spring housing market
Prices up, sales down in early spring housing market
 Area property deed transfers, April 18
Area property deed transfers, April 18
 Tea Guys of Whately owes $2M for breach of contract, judge rules
Tea Guys of Whately owes $2M for breach of contract, judge rules
Arts & Life

Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28
A lot can change in 20 years: Presidents and other politicians come and go, new cultural fads and technologies emerge, clothing styles morph, and music and movies take on different dimensions.In these parts, one tradition hasn’t changed. Since 2005,...
Obituaries
 Maryann Burke
Maryann Burke
Hatfield, MA - Maryann Burke (DeMatto), beloved wife, mother and Nonna, passed away on April 19, 2024, with her loving husband by her side. Maryann was born in Holyoke, MA on September 3, 1944, to the late Joseph and Emelia DeMatto. ... remainder of obit for Maryann Burke
 Crystal L. Bergeron
Crystal L. Bergeron
Crystal L Bergeron Easthampton, MA - Crystal L Bergeron, 39, of Easthampton sadly left us as she passed away peacefully at home on April 11th, 2024. She was born July 18, 1984, to Roger J Bergeron and Darlene J Bergeron. Crystal had the ... remainder of obit for Crystal L. Bergeron
 Richard A. Weber
Richard A. Weber
Richard A Weber Shutesbury, MA - In the earliest hour of Saturday, April 13, 2024, surrounded by the tremendous love of his family, Richard Weber, 60, gently left this world. Rich leaves behind an amazing group of folks who loved him wh... remainder of obit for Richard A. Weber
 Daniel James Moriarty
Daniel James Moriarty
Granby, MA - Daniel J. Moriarty, 66, passed away unexpectedly on April 14, 2024. He was born January 12, 1958 in Holyoke, MA. to the late Donald and Marie Moriary. Daniel grew up in South Hadley and graduated from South Hadley High Scho... remainder of obit for Daniel James Moriarty

 Amherst regional district towns seek middle ground on school increase
Amherst regional district towns seek middle ground on school increase
 Prescription drug take back day set for Saturday in 15 communities in Hampshire, Franklin counties
Prescription drug take back day set for Saturday in 15 communities in Hampshire, Franklin counties
 Area briefs: Suicide prevention forum; ‘American Symphony’ screening; Zonta grant awards
Area briefs: Suicide prevention forum; ‘American Symphony’ screening; Zonta grant awards
 Senate may reform trio of consumer laws: competitive electricity, used car sales, heating oil leaks
Senate may reform trio of consumer laws: competitive electricity, used car sales, heating oil leaks
 Granby man admits guilt, gets 2½ years in vehicular homicide
Granby man admits guilt, gets 2½ years in vehicular homicide
 South Hadley residents will pay more for trash, wastewater rates next fiscal year
South Hadley residents will pay more for trash, wastewater rates next fiscal year
 Area briefs: Transhealth to celebrate 3 year; Holyoke to plant tree at museum; Documentary film about reparations focus of Unitarian talk
Area briefs: Transhealth to celebrate 3 year; Holyoke to plant tree at museum; Documentary film about reparations focus of Unitarian talk
 Leverett Town Meeting voters will decide cease-fire call, budgets, town elections
Leverett Town Meeting voters will decide cease-fire call, budgets, town elections
 UMass set to inaugurate Javier Reyes as chancellor on Friday
UMass set to inaugurate Javier Reyes as chancellor on Friday
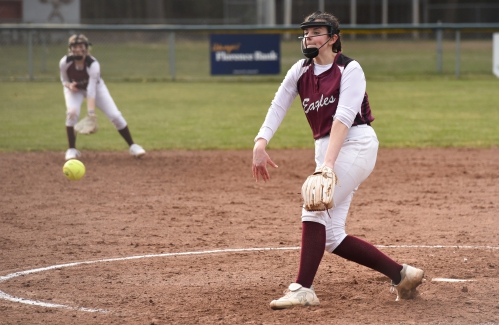
 Softball: Offense erupts as Hampshire Regional thumps East Longmeadow 15-3 to get back in win column
Softball: Offense erupts as Hampshire Regional thumps East Longmeadow 15-3 to get back in win column Owen Dawson notches 200th career point for South Hadley boys lacrosse team
Owen Dawson notches 200th career point for South Hadley boys lacrosse team South Hadley’s Lauren Marjanski signs National Letter of Intent to play soccer at Siena College
South Hadley’s Lauren Marjanski signs National Letter of Intent to play soccer at Siena College Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many
Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many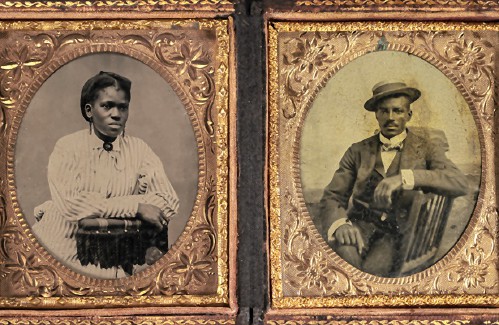 Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history Earth Matters: From Big Sits to Birdathons: Birding competitions far and near
Earth Matters: From Big Sits to Birdathons: Birding competitions far and near Speaking of Nature: Indulging in eye candy: Finally, after such a long wait, it’s beginning to look like spring is here
Speaking of Nature: Indulging in eye candy: Finally, after such a long wait, it’s beginning to look like spring is here
