
Organizers ramping up for bigger Northampton Pride this year
NORTHAMPTON — Under new organizers and a nine-week planning schedule, Pride returned to the queer capital of Northampton last year after a three-year hiatus, and it’s back to stay.Hampshire Pride, the nonprofit that revived Pride in the Pioneer Valley...

Crocker School kids draw on historical picture books for library banner project
AMHERST — An unfolded brown paper bag is being transformed, through use of crayons, pencils and paint markers, into a banner showcasing an acclaimed American naturalist, artist and academic.“I think Anna Comstock was very impressive in her work,” says...
Most Read
 Two men dump milk, orange juice over themselves at Amherst convenience store
Two men dump milk, orange juice over themselves at Amherst convenience store
 Three Amherst Regional Middle School counselors absolved of Title IX offenses
Three Amherst Regional Middle School counselors absolved of Title IX offenses
 Springfield man charged with murder in Holyoke stabbing
Springfield man charged with murder in Holyoke stabbing
 Lawmakers, Jewish groups accuse Massachusetts Teachers Association of bias
Lawmakers, Jewish groups accuse Massachusetts Teachers Association of bias
 ‘Our hearts were shattered’: Moved by their work in Mexico soup kitchen, Northampton couple takes action
‘Our hearts were shattered’: Moved by their work in Mexico soup kitchen, Northampton couple takes action
 Hadley’s Brad Mish, Northampton’s Elianna Shwayder top Hampshire County finishers at 128th Boston Marathon
Hadley’s Brad Mish, Northampton’s Elianna Shwayder top Hampshire County finishers at 128th Boston Marathon
Editors Picks
 A Look Back: April 17
A Look Back: April 17
 Spring brings new art: A look at what's on tap in April at selected local galleries
Spring brings new art: A look at what's on tap in April at selected local galleries
 News Briefs: Roadwork in Plainfield; bake sale in Hadley
News Briefs: Roadwork in Plainfield; bake sale in Hadley
 Three Amherst Regional Middle School counselors absolved of Title IX offenses
Three Amherst Regional Middle School counselors absolved of Title IX offenses
Sports

Jiri Smejkal gets 1st goal, Senators beat Bruins 3-1 in regular-season finale
BOSTON — Jiri Smejkal scored his first career goal midway through the second period and Jakob Chychrun scored less than a minute later as the Ottawa Senators beat the Boston Bruins 3-1 on Tuesday night in the regular-season finale for both teams.Artem...
 High schools: Belchertown, Easthampton split dual track meet (PHOTOS)
High schools: Belchertown, Easthampton split dual track meet (PHOTOS)
 High school ultimate preview: Amherst, Northampton hoping for big seasons
High school ultimate preview: Amherst, Northampton hoping for big seasons
 UMass basketball: Matt Cross reportedly enters transfer portal
UMass basketball: Matt Cross reportedly enters transfer portal
Opinion

Rachel Vigderman: Area women ending silence over weaponization of rape
I want to commend Sara Weinberger for her column “The appalling silence over the atrocities of October 7th” [Gazette, April 15]. As co-president of the Northampton/Amherst Chapter of Hadassah I would like to report that area residents, along with...
 Maggie Baumer: Access to prosthetics and orthotics for physical activity a right, not a privilege
Maggie Baumer: Access to prosthetics and orthotics for physical activity a right, not a privilege
 Toni Doherty: 2020s essential workers: Oxymoron?
Toni Doherty: 2020s essential workers: Oxymoron?
 Timmon Wallis: More funding for Ukraine not the answer
Timmon Wallis: More funding for Ukraine not the answer
 Columnist Razvan Sibii: How to welcome a refugee family into your community
Columnist Razvan Sibii: How to welcome a refugee family into your community

Business

Area property deed transfers, April 18
AMHERST 44 Chapel Rd, $560,750, B: Kristin M. Flewelling and Christine L. Larson, S: Paul A. Schroeder and Maria Monasterios BELCHERTOWN 203 South St, $507,150, B: Glenna J. Young, S: M & F Land Dev LLC 45 West St, $200,000, B: Serenity Ft and...
 Tea Guys of Whately owes $2M for breach of contract, judge rules
Tea Guys of Whately owes $2M for breach of contract, judge rules
Arts & Life

Speaking of Nature: Indulging in eye candy: Finally, after such a long wait, it’s beginning to look like spring is here
I have just about reached the end of my patience with the winter of 2024. I realize that this may sound a bit strange, especially because we are now in the beginning of spring, but those of us who bore the brunt of the April snowstorm may sympathize...
Obituaries
 Geraldine Packard
Geraldine Packard
Northampton, MA - Geraldine Packard, 87, passed away at her home in Northampton on April 13, 2024. Born to Curtis and Mildred (Smith) Chase on September 23, 1936 in Wolfeboro, New Hampshire... remainder of obit for Geraldine Packard
 Russell E. Lent Sr.
Russell E. Lent Sr.
[IMAGE]Russell E. Lent, Sr. Easthampton, MA - Russell Eugene Lent, Sr. 89, longtime resident of Easthampton, passed away peacefully on Friday April 12, 2024, at his home. Born in Coshocton, ... remainder of obit for Russell E. Lent Sr.
 Floris Cathelineaud
Floris Cathelineaud
Amherst, MA - On April 14, 2024, Floris Cathelineaud Diaz (Abu) was called to Eternal Rest peacefully at home, surrounded by family and friends, at age 96. She is survived by her daughters, Dr. ... remainder of obit for Floris Cathelineaud
 Judith Fuhring Seelig
Judith Fuhring Seelig
Amherst, MA - Judith Fuhring Seelig was born April 19, 1950 and passed away on October 21, 2023 Family and friends invite you to a Celebration of Life in memory of our beloved Judith wh... remainder of obit for Judith Fuhring Seelig

 Mass. saw nearly 200 percent rise in antisemitic incidents last year
Mass. saw nearly 200 percent rise in antisemitic incidents last year
 Three finalists named for Ryan Road School principal in Northampton
Three finalists named for Ryan Road School principal in Northampton
 Prices up, sales down in early spring housing market
Prices up, sales down in early spring housing market
 Guest columnist Jim Palermo: Beware the zeitgeist! It’s bad for our kids
Guest columnist Jim Palermo: Beware the zeitgeist! It’s bad for our kids
 Boyfriend accused in slaying of Hampden sheriff’s assistant, former legislator’s top aide
Boyfriend accused in slaying of Hampden sheriff’s assistant, former legislator’s top aide
 Revised plan to combat bullying in Amherst regional schools questioned
Revised plan to combat bullying in Amherst regional schools questioned
 Wheeling for Healing returns to South Deerfield to raise money for cancer treatment
Wheeling for Healing returns to South Deerfield to raise money for cancer treatment
 Sadiq to leave Amherst middle school principal role
Sadiq to leave Amherst middle school principal role
 Northampton seeks bids to redevelop former Registry of Deeds property
Northampton seeks bids to redevelop former Registry of Deeds property
 High school: Northampton softball slugs past Mahar for season's first victory (PHOTOS)
High school: Northampton softball slugs past Mahar for season's first victory (PHOTOS) Recognizing an ‘inspiring force’: City business owner honored with Black Excellence award
Recognizing an ‘inspiring force’: City business owner honored with Black Excellence award Consumer Corner with Anita Wilson: A two-day reprieve in tax filing deadline offers time for tips
Consumer Corner with Anita Wilson: A two-day reprieve in tax filing deadline offers time for tips Sublime Systems lands $87M federal award for low-carbon cement plant in Holyoke
Sublime Systems lands $87M federal award for low-carbon cement plant in Holyoke Weekly Food Photo Contest: This week’s winner: Nicholas Horton of Northampton
Weekly Food Photo Contest: This week’s winner: Nicholas Horton of Northampton What does freedom look like today? On view at Williams College, seven Black American artists interpret the meaning of emancipation
What does freedom look like today? On view at Williams College, seven Black American artists interpret the meaning of emancipation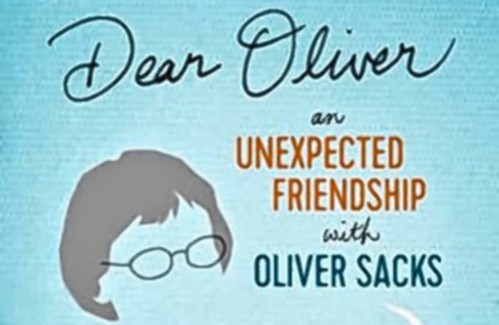 Book Bag: ‘Dear Oliver: An Unexpected Friendship With Oliver Sacks’ by Susan B. Barry; ‘Benjy’s Messy Room’ by Barbara Diamond Goldin
Book Bag: ‘Dear Oliver: An Unexpected Friendship With Oliver Sacks’ by Susan B. Barry; ‘Benjy’s Messy Room’ by Barbara Diamond Goldin Only Human with Joan Axelrod-Contrada: To journal or not to journal: Advice for when journaling feels like it’s holding you back
Only Human with Joan Axelrod-Contrada: To journal or not to journal: Advice for when journaling feels like it’s holding you back
