Latest News
 Hadley planners advance battery storage bylaw
Hadley planners advance battery storage bylaw
 Gun buyback event collects 195 unwanted firearms
Gun buyback event collects 195 unwanted firearms

Fearful Belchertown residents blame stray bullets on nearby gun club, appeal to town for help
BELCHERTOWN — Jake Hulseberg won’t let his children play on the swing set he built them in their backyard on Mountain View Drive because of bullets that shattered glass doors on two houses on the street.Instead, Hulseberg keeps his kids in the front...

Quabbin region studied for MWRA expansion
As House Democrats eye the expansion of its public drinking water service area, the Massachusetts Water Resources Authority (MWRA) is considering whether the communities where that water comes from should finally get to reap the benefits of the...
Most Read
 Holyoke man finds bear paw in his yard
Holyoke man finds bear paw in his yard
 Boyfriend accused in slaying of Hampden sheriff’s assistant, former legislator’s top aide
Boyfriend accused in slaying of Hampden sheriff’s assistant, former legislator’s top aide
 Three finalists named for Ryan Road School principal in Northampton
Three finalists named for Ryan Road School principal in Northampton
 Developer pitches new commercial building on Route 9 in Hadley
Developer pitches new commercial building on Route 9 in Hadley
 Two men dump milk, orange juice over themselves at Amherst convenience store
Two men dump milk, orange juice over themselves at Amherst convenience store
 Sadiq to leave Amherst middle school principal role
Sadiq to leave Amherst middle school principal role
Editors Picks
 New federal mandate requires informed consent for sensitive exams
New federal mandate requires informed consent for sensitive exams
 Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
 Area Briefs: Northampton kicks off Earth Day celebrations
Area Briefs: Northampton kicks off Earth Day celebrations
 The Beat Goes On: Album release shows by Barnstar! and Lisa Bastoni, a Young@Heart Chorus concert with new special guests, and more
The Beat Goes On: Album release shows by Barnstar! and Lisa Bastoni, a Young@Heart Chorus concert with new special guests, and more
Sports

Boys lacrosse: Landon Andre, Nico St. George help Belchertown hold off Amherst 11-9 (PHOTOS)
BELCHERTOWN — After a quick 3-1 flurry from the Amherst boys lacrosse team erased Belchertown’s three-goal lead, the Orioles clung to a 9-8 advantage early in the fourth quarter on Thursday afternoon.Somebody had to step up for Belchertown to put a...
 The Real Score: Curveballs and casinos rarely save cities
The Real Score: Curveballs and casinos rarely save cities
 Baseball: Chicopee Comp strikes early, takes down Amherst (PHOTOS)
Baseball: Chicopee Comp strikes early, takes down Amherst (PHOTOS)
 Florence’s Gabby Thomas gearing up for 2024 Paris Olympics
Florence’s Gabby Thomas gearing up for 2024 Paris Olympics
Opinion

Bridget Miller: Why walkability is the pathway to a healthy Amherst community
Picture a quiet rural town where the charm of winding roads and open spaces should invite pleasant walks and friendly encounters. Yet, instead of a stroll, residents navigate treacherous paths and dodge traffic on roads devoid of sidewalks or safe...
 Guest columnist Mariel E. Addis: Under seige from all sides
Guest columnist Mariel E. Addis: Under seige from all sides
 Julia Riseman: Join Friends of Northampton Trails
Julia Riseman: Join Friends of Northampton Trails
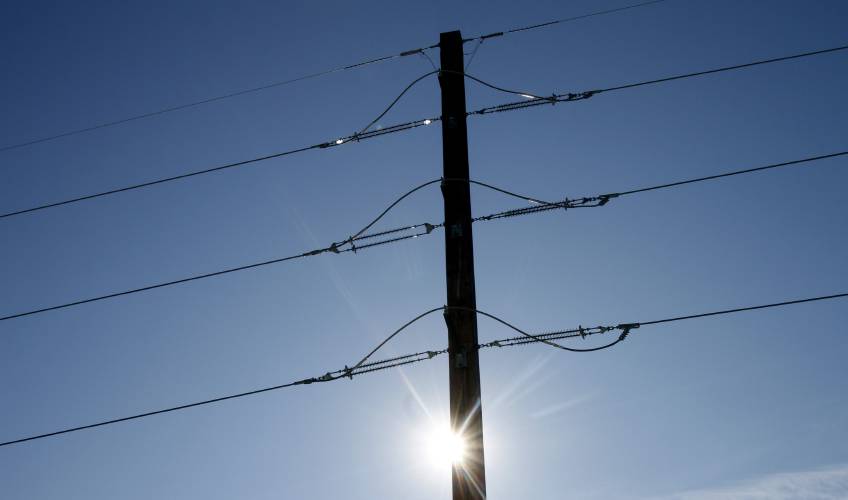 Justine McCarthy and Ed Lamoureux: Political will needed to benefit from new power line technology
Justine McCarthy and Ed Lamoureux: Political will needed to benefit from new power line technology
 Shelly Berkowitz: More examples of corporate greed
Shelly Berkowitz: More examples of corporate greed

Business

Petition to block auto dealership on King Street falters in Northampton
NORTHAMPTON — A joint meeting between the Northampton City Council’s Committee on Legislative Matters and the city’s Planning Board heard public comments on a petition to ban further automobile dealerships near the city’s downtown, an issue that...
 Flair and flavor: Couple draws on European, regional travel and food expertise to bring gourmet Aster + Pine Market to Amherst
Flair and flavor: Couple draws on European, regional travel and food expertise to bring gourmet Aster + Pine Market to Amherst
 Prices up, sales down in early spring housing market
Prices up, sales down in early spring housing market
 Area property deed transfers, April 18
Area property deed transfers, April 18
 Tea Guys of Whately owes $2M for breach of contract, judge rules
Tea Guys of Whately owes $2M for breach of contract, judge rules
Arts & Life

Earth Matters: From Big Sits to Birdathons: Birding competitions far and near
A few months ago, headlines flared that Peter Kaestner had seen his 10,000th bird species. This could have been anticlimactic, as Kaestner has been renowned for years among birders for traveling worldwide and seeing more species than anyone.However,...
Obituaries
 Garry Tudryn
Garry Tudryn
[IMAGE]GARRY TUDRYN HATFIELD, MA - Garry Morrison Tudryn, 67 of West Street in Hatfield, passed away April 13, 2024 at the Care One Nursing and Rehab Center in Northampton. Born in Northampt... remainder of obit for Garry Tudryn
 Jacques Ben Abbes
Jacques Ben Abbes
HADLEY, MA - Jacques Ben Abbes, leaves his wife, Ngoc Anh Tran. Children; Vincent Tran (Nhu Nguyen) and Jacqueline Ben Abbes (Victor Loye) Grandchildren, Benjamin and Scott Tran. CALLIN... remainder of obit for Jacques Ben Abbes
 Geraldine Packard
Geraldine Packard
Northampton, MA - Geraldine Packard, 87, passed away at her home in Northampton on April 13, 2024. Born to Curtis and Mildred (Smith) Chase on September 23, 1936 in Wolfeboro, New Hampshire... remainder of obit for Geraldine Packard
 Russell E. Lent Sr.
Russell E. Lent Sr.
[IMAGE]Russell E. Lent, Sr. Easthampton, MA - Russell Eugene Lent, Sr. 89, longtime resident of Easthampton, passed away peacefully on Friday April 12, 2024, at his home. Born in Coshocton, ... remainder of obit for Russell E. Lent Sr.

 State: South Hadley’s fiber-optic revenues not public records
State: South Hadley’s fiber-optic revenues not public records
 Man granted parole for his role in the 2001 stabbing deaths of 2 Dartmouth College professors
Man granted parole for his role in the 2001 stabbing deaths of 2 Dartmouth College professors
 Developer lands $400K loan for affordable housing project in Easthampton mill district
Developer lands $400K loan for affordable housing project in Easthampton mill district
 Columnist Johanna Neumann: Reaping the rewards of rooftop solar
Columnist Johanna Neumann: Reaping the rewards of rooftop solar
 Amherst Fire Chief Walter ‘Tim’ Nelson to retire in June
Amherst Fire Chief Walter ‘Tim’ Nelson to retire in June
 First look at how little Amherst’s police alternative being used called troubling
First look at how little Amherst’s police alternative being used called troubling
 High schools: Offense on fire for Granby girls lacrosse in 20-2 win over McCann Tech
High schools: Offense on fire for Granby girls lacrosse in 20-2 win over McCann Tech Speaking of Nature: Indulging in eye candy: Finally, after such a long wait, it’s beginning to look like spring is here
Speaking of Nature: Indulging in eye candy: Finally, after such a long wait, it’s beginning to look like spring is here Weekly Food Photo Contest: This week’s winner: Nicholas Horton of Northampton
Weekly Food Photo Contest: This week’s winner: Nicholas Horton of Northampton What does freedom look like today? On view at Williams College, seven Black American artists interpret the meaning of emancipation
What does freedom look like today? On view at Williams College, seven Black American artists interpret the meaning of emancipation Spring brings new art: A look at what's on tap in April at selected local galleries
Spring brings new art: A look at what's on tap in April at selected local galleries 
